Pumping Blood
Today, we pump blood. The University of Houston's College of Engineering presents this series about the machines that make our civilization run, and the people whose ingenuity created them.
Christiaan Barnard made history in Cape Town, South Africa, in 1967, with the first human heart transplant. It kept a dying man alive for another eighteen days. Now, in America alone, such operations annually keep more than 2000 people alive for years.
Fifteen years later, the first artificial heart was implanted in Barney Clark. It kept him alive for a scant sixteen weeks. And, even at this writing in 2007, artificial hearts remain temporary. They're still a stopgap for patients awaiting human replacement hearts. Well, maybe that'll change before this reaches reruns.
Messing with the human heart was very radical in the mid-20th century. Even the most elementary heart surgery was still in its infancy. And replacement hearts -- real or artificial -- really pushed the envelope. They pushed credulity itself.
Several 19th-century doctors had sutured stab wounds to patients' hearts. Two were done successfully by black surgeon Daniel Dalton in St. Louis -- one in 1889, another two years later.
But to do more elaborate heart surgery, one had to keep a patient alive with the heart stopped. The great puzzle was, if a patient were temporarily taken off his own heart, how could he get the oxygen-rich blood needed to survive the surgery? Well, it clearly had to come from some form of external heart.
In the 1930s, Charles Lindbergh and Alexis Carrel developed an external pump to reoxygenate and recirculate a patient's blood during surgery. It was only marginally successful, but it sent an important message when it made the cover of Time magazine. Obviously the more important form of artificial heart would be the temporary one that served patients during surgery.
Now an article in New Science magazine celebrates a turning point in cardiac surgery. In 1954, Walter Lillehei at the University of Minnesota had come to a startling realization. It was that we can live on a lot less blood than our hearts pump. Perhaps a human being could serve as the external pump.
When a thirteen-month old child showed up with a hole in the wall between two heart chambers, Lillehei (to the horror of other doctors) used the boy's father's heart to pump blood for them both. He simply shunted a portion of the father's blood through the infant while he operated. It worked. Alas, soon after, the child caught pneumonia and died. But Lillehei did 27 more heart surgeries, and most of them succeeded.
After Lillehei, regular heart surgery could be seen as plausible. Spurred by his successes, inventors finally produced a workable external heart pump the next year. And we all have friends who've been saved by the resulting surgeries. So I give you this little-known hero of heart surgery -- hardly a household name, but his insight and action were pivotal. Now the whole business became commonplace. After Lillehei, an odd line by Longfellow takes on new meaning. He wrote:
Ah, nothing is too late,
Till the tired heart shall cease to palpitate.
I'm John Lienhard, at the University of Houston, where we're interested in the way inventive minds work.
S. Pain, One Heart Beating for Two. New Science, July 28-August 3, 2007, pp. 50-51.
For more on Lillehei and Barnard, respectively, see:
https://en.wikipedia.org/wiki/C._Walton_Lillehei
https://en.wikipedia.org/wiki/Christiaan_Barnard
To read about heart transplant statistics, heart transplants, artificial hearts, and cardiac surgery, respectively, see:
https://en.wikipedia.org/wiki/Heart_transplantation
https://en.wikipedia.org/wiki/Artificial_heart
https://en.wikipedia.org/wiki/Cardiac_surgery
The Longfellow line is from Stanza 22 of Morituri Salutamus.
I am grateful to Dr. Stanley J. Reiser, George Washington University Medical School, for his valuable counsel.
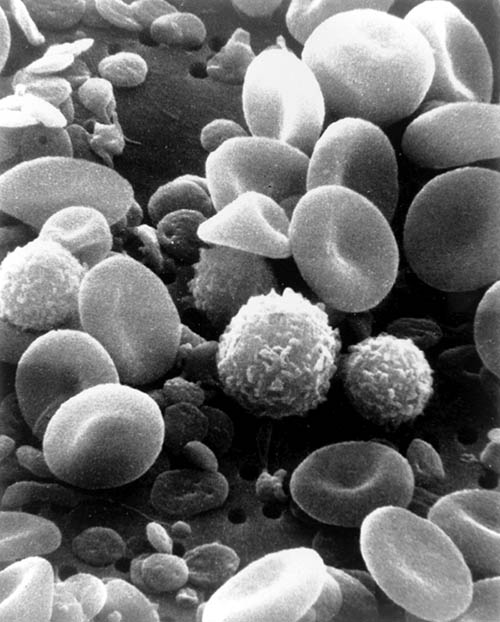
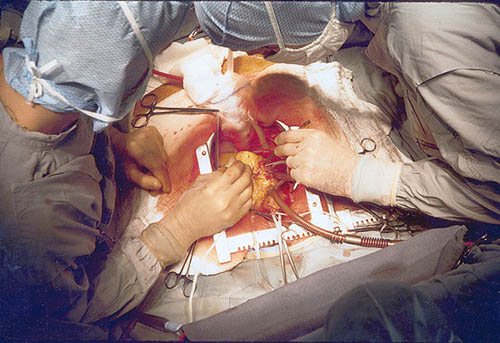
Images below, courtesy of Wikipedia: Top, a scanning electron microscope photo of human blood, with its many components, suggests the delicacy with which it must be handled when it is recirculated. Bottom, two surgeons doing a coronary artery bypass.